Harvard Study Rewrites the Smoke Screen: Cannabis Far Less Harmful to Lungs Than Tobacco
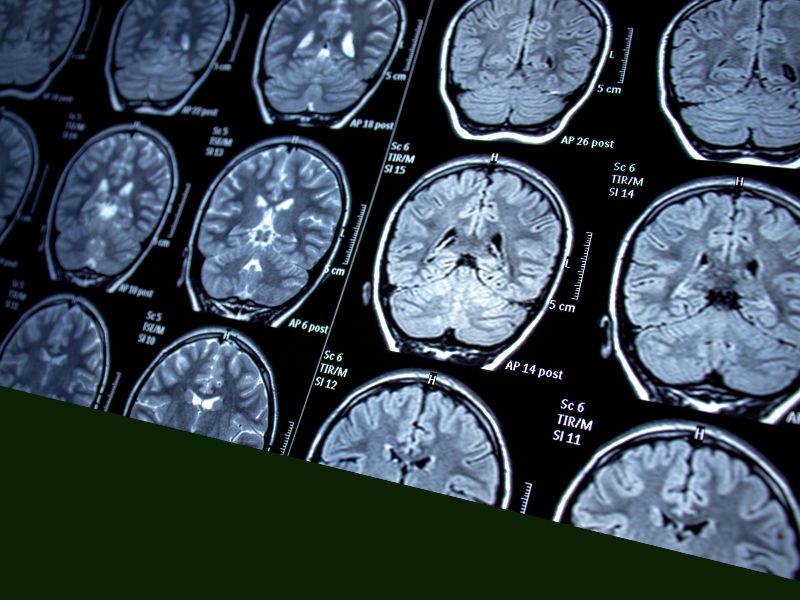
A landmark investigation from Harvard Medical School, recently published in Current Problems in Diagnostic Radiology, has delivered a clear verdict: exclusive cannabis smoking does not carry the same pulmonary risks as tobacco. By analyzing high-resolution CT scans of 285 carefully matched participants—89 non-smokers, 97 cigarette smokers, and 99 marijuana‐only smokers—the researchers uncovered dramatic differences in lung health. While more than six in ten tobacco users showed visible emphysema on imaging, a mere 4 percent of cannabis smokers exhibited any emphysematous changes. Furthermore, tobacco smokers manifested greater lung hyperinflation and nearly double the rate of coronary artery calcifications compared to their marijuana-using peers.
Rigorous Methods Validate the Findings
This study’s strength lies in its dual quantitative–qualitative approach. Total lung volume (TLV) was measured to detect subtle differences in hyperinflation, while blinded thoracic radiologists assessed CT scans for emphysema, ground‐glass opacities, and bronchial wall changes. Despite slight age differences among groups, results were statistically robust: tobacco smokers had significantly higher TLV and centrilobular emphysema rates (62 percent), whereas marijuana smokers closely mirrored non‐smokers. The distinct patterns observed suggest that the unique chemical composition of cannabis smoke—lacking many of tobacco’s combustion byproducts—spares the delicate alveolar structures that, once damaged, lead to chronic lung disease.
Broader Health and Policy Ramifications
These findings reinforce a growing consensus: equating cannabis with tobacco in public health policy is scientifically unfounded. NORML deputy director Paul Armentano underscores the absurdity of Congress listing cannabis among the most dangerous substances while leaving deadly tobacco unregulated at the federal level. This research adds momentum to calls for federal rescheduling of cannabis, which would unlock funding for comprehensive long-term studies and ensure that regulatory stance keeps pace with scientific reality.
Michigan’s Harm Reduction Model: Vaporization and Beyond
Michigan, one of the nation’s most forward-thinking states in cannabis regulation, already permits a broad array of vaporizable products. Vaporization—a process heating cannabis below combustion thresholds—has been validated in clinical trials as a “safe and effective” delivery system, dramatically reducing exposure to harmful tars and gases. Expanding access to vaporizers, alongside robust patient education on dosing and device maintenance, offers a blueprint for other jurisdictions seeking to embrace harm reduction. As policymakers weigh smoke-free lounges and home-use guidelines, Michigan’s model demonstrates how science can shape smarter regulations that protect public health.
Implications for Patients and Healthcare Providers
For clinicians treating chronic pain, PTSD, or cancer‐related symptoms, this study provides reassuring data when discussing inhaled cannabis with patients. While oral and topical formulations remain important options, the choice to smoke cannabis exclusively should not automatically raise red flags about emphysema or COPD risk. Physicians can now counsel patients on respiratory safety more confidently, emphasizing moderate use and considering vaporization to maximize benefits while mitigating any residual smoke exposure.
Economic and Social Equity Considerations
Beyond health, these findings carry economic and social justice weight. Reduced respiratory harm supports broader adult-use legalization, which in turn generates tax revenue for public health initiatives and community reinvestment. Equitable licensing and support for small growers—often overlooked in legacy markets—ensure that those historically marginalized in drug enforcement can participate in a booming industry. Aligning cannabis policy with scientific evidence not only safeguards lungs but also promotes social equity and economic inclusion.
Looking Ahead: Research Needs and Hope for Reform
While this CT-based study offers critical insights, questions remain about long-term effects, especially among heavy or aging users. Future research should explore interactions between cannabis smoke and preexisting lung conditions, genetic susceptibility to smoke‐related damage, and comparisons with emerging inhalation technologies. Nonetheless, these results mark a turning point: cannabis is no tobacco twin in lung risk. As Michigan and other states refine their regulatory frameworks, embracing evidence-based reforms will pave the way for a regulatory environment that truly balances public health, patient choice, and social justice—heralding a new era where cannabis policy finally catches up with the science.